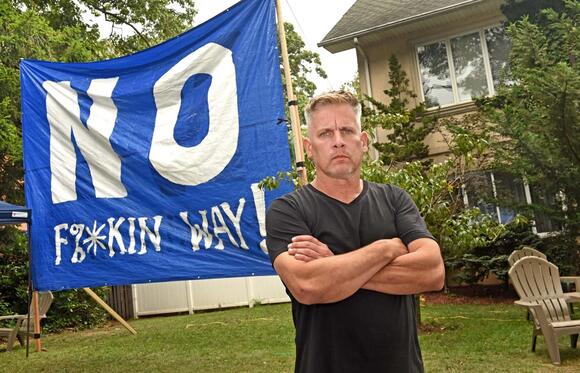
A newborn baby receives oral antibiotics, one of many contributing
factors to alterations in the gut microbiome that modulates immunity.
(Shutterstock)
https://www.theepochtimes.com/health/is-the-goliath-in-autism-research-about-to-fall-5427600
Autism is increasing at rapid rates, and researchers may be looking in the wrong places for the answer as to why.
An extensive meta-analysis of 25 autism studies could shift the focus
of research into the cause of autism from genetics to environmental
triggers. That shift could open up new, revolutionary avenues for
potential treatments.
The research ties the disorder to changes in the gut microbiome, a
community of microbes that live in the colon and are responsible for
creating metabolites and other compounds crucial to our health and
wellness.
Many influences outside of the human body are killing these
beneficial microbes, which aren’t genetically part of us but live in
symbiosis with humans. The new study, published June 26 in Nature Neuroscience,
has linked autism spectrum disorders (ASD) to a distinct microbial
signature that’s dysbiotic, or unnaturally out of balance. As in an
ecosystem, too much of certain problematic species can destroy the
overall ecology or lead to problematic consequences, such as too many of
certain metabolites and not enough of others.
Meanwhile, autism rates are increasing at a speed that defies
improved screening and diagnostic practices, as well as genetic
patterns. The Centers for Disease Control released statistics in April that show the latest autism rate was 1 in 36 children in 2020, up from 1 in 44 in 2018, and 1 in 150 in 2000.
Taken together, the evidence suggests that it’s time to direct
resources to pinpointing exactly what it is in our environment that
appears to “turn on” autism development, according to doctors who are
treating patients with ASD.
“Genetic diseases aren’t responsible for epidemics,” Dr. Arthur Krigsman, a
specialist who treats children with ASD around the world, told The
Epoch Times. “There’s something in the environment that’s triggering a
gene that otherwise would be silent. There is no gene responsible for an
epidemic.”
Our genes are wound up tightly in DNA spirals—many of them never
being used—similar to blueprints that never make their way to the
manufacturer. But cues in our environment can trigger epigenetic
processes that trigger some genes to get turned on or others to get
turned off, dramatically changing our likelihood of developing certain
diseases or attributes.
The new research suggests that autism is linked to epigenetic
triggers, which are influenced by the microbiome and modifiable over the
course of our lifetime.
Researchers will undoubtedly keep trying to tease out some of the genetic links to the neurological disorder, which is largely diagnosed in childhood. Autism has been connected to more than 100 genes so far. But the puzzle has gotten more complex with environmental associations that seem to keep growing. And the heterogeneity of ASD makes it impossible to accuse one single factor as the cause.
The Epigenetic Nature of Autism
Many doctors believe that autism arises when “toxic” environmental
pressures are applied and trigger epigenetic changes, Dr. Mark Cannon, a
professor at Northwestern University, told The Epoch Times.
Toxicities can be biological and chemical but also emotional and
social, and they can interfere with physiology. Examples include air
pollutants, artificial food ingredients, glyphosate, medications,
viruses, and even stress, which causes a biochemical cascade of changes
in the body. All exert influence by changing the microbiome.
This community of trillions of bacteria, viruses, and fungi is
responsible for breaking down food into metabolites, especially
short-chain fatty acids (SCFAs) that communicate vital information to
the whole body to perform digestive, neurological, and other functions.
The main roles of these gut bugs are metabolism, nutrient absorption, and immune function.
Microbiomes are constantly in flux, and it’s becoming impossible to
define exactly what a healthy microbiome looks like because our
industrial world has already altered our microbiome in severe ways.
We’re only learning how to study them in detail now. That said, patterns
are emerging, and studies are offering powerful clues about how
diseases are linked to certain microbiome patterns.
Dr. Cannon pointed to an autism study published in 2012 in Microbial Ecology in Health and Disease that showed the epigenetic nature of autism. Rats were given SCFAs from a subject with autism.
The rats displayed abnormal motor movements, repetitive behavior,
cognitive deficits, impaired social interactions, and other traits
common in autism. The brain tissue of treated rats also showed
neurochemical changes—such as innate neuroinflammation, increased
oxidative stress, and glutathione depletion—consistent in patients with
ASD.
“Conceptually, it is the author’s opinion that the pathophysiology of
ASDs may be more completely understood as being similar to conditions
such as ethanol intoxication, or diabetes, and the resultant complex
interactions between diet, genetics, metabolism, host microbiome, and
behavior, that are well known to exist in these treatable disorders
throughout the life cycle,” Dr. Derrick F. MacFabe, the study’s author,
wrote.
He suggested that SCFAs are the trigger of ASD or ASD behavior. SCFAs are derived
from the fermentation of nondigestible polysaccharides, such as
resistant starches and dietary fibers. Among their physiological
functions, SCFAs are important to intestinal epithelial cell growth,
which protects the gut barrier, and to inflammation regulation.
“Yes, you can turn autism on,” Dr. Cannon said. “I can’t tell you how
many times I’ve sat at a conference and heard, ‘I always thought that
was genetic,’ when in fact the data has never supported that.”
Disempowerment of Genetics
Focusing too much on genetics as the cause of disease can be a
detriment to important avenues of research and treatment, and can
discourage families with autistic children. Wholeheartedly embracing
genetics leaves them powerless, Dr. Armen Nikogosian told The Epoch
Times.
In that case, for people with autism and their families, the only
option is to manage the symptoms with pharmaceuticals, he said.
Dr. Nikogosian shifted his entire medical practice in 2010 after one of his sons was diagnosed with autism.
“That’s the message I got. That’s the message a lot of parents get,”
he said. “They’re entrenched in this idea that there’s this genetic
cause involved in this.”
Dr. Nikogosian’s goal is to help parents who want to address the root
causes of the disorder with a more holistic model of care that doesn’t
rely on drug management of symptoms.
He said that the development of other treatments has stagnated
because of the broad denial that environmental factors are involved.
“There’s absolutely, positively, no question there’s a massive input from environmental exposures,” Dr. Nikogosian said.
Some exposures that he explores with patients are heavy metal and
mold exposures, multiple infections, and vaccines. Clarifying,
quantifying, and understanding the contributions of environmental
exposures are important, as it opens doors to novel treatments.
Some Environmental Influences Are Known
Autism researcher James Adams said that many hypothesized risk factors continue to be validated by research. In a recent study that
he conducted on a small cohort of children with autism, he discovered
that common themes were prevalent throughout research.
“It turns out mothers of kids with autism consumed lower fiber, less
fiber than moms of typical kids. That’s important because fiber is a
very important food for some gut bacteria,” he said. “You inherit most
of your microbiome from your mother.”
A 2021 study in Frontiers in Immunology
found that there’s an uptick of SCFA production in pregnant women
associated with fetal immune system development. The study connected
breastfed babies with more diverse and robust microbiome development.
Mr. Adams said that his research and other studies have shown
formula-fed babies and those with increased use of oral antibiotics are
more likely to be diagnosed with autism. Early delivery
is also a risk factor for autism; the Frontiers article noted that
premature birth tends to impact microbiome development. Babies delivered
vaginally also have more diverse microbes and lower rates of illness
than those born via cesarean section.
Other common, pregnancy-related factors for ASD include maternal
obesity, maternal diabetes, and complications associated with trauma,
ischemia, and hypoxia, according to data reported in Neuron in 2018.
A study recently published in Psychological and Cognitive Sciences
that included 450 mother-child pairs noted that at age 2, children
whose moms had experienced adversity as children had altered
microbiomes. Other issues that moms can experience that appear to impact
their babies’ microbiomes are antibiotic use and infections.
The pathway between the microbiome and autism has gained several
validating findings, making it difficult to deny as a causal factor. In a
perfect world, physicians say, it should lead to major changes in
clinical settings.
“You always want to know the cause, because if you know the cause,
you can stop the disease,” Dr. Krigsman said. “Stop looking for a gene
that probably doesn’t exist and won’t be found. Try to find the cause,
and then remedy that, remove that.”
Why Cause Matters
Microbiologist Kiran Krishna told The Epoch Times that what appears
to be coming is similar to the global realization that smoking was
causing cancer.
The tobacco industry eventually couldn’t stop the number of small,
cumulative studies that clearly documented the link. Mr. Krishna said
that the same thing is happening regarding the connection between the
microbiome and autism, and the new meta-analysis is important because it
can help other researchers attract grants and funding to look more
intentionally at microbes and their environmental influences.
“Before this, we had smoke indicating the microbiome was involved in
autism, and now we have fire,” Rob Knight, the director of the Center
for Microbiome Innovation at the University of California–San Diego and a
study co-author, said in a statement.
There’s still a debate about whether the disease is driving dysbiosis, or the other way around. A 2021 study published in Cell concluded
that dietary preferences, or restrictive eating that’s common among
children with autism, is what causes changes in the microbiome. “We
caution against claims that the microbiome has a driving role in ASD,”
the researchers wrote.
Mr. Krishna suspects that the longitudinal data from the new study
will help settle any lingering doubts as to whether the microbiome is a
driver of ASD.
“We’re getting there because there are so many researchers globally
that are interested in the microbiome,” he said. “We’re hitting that
wave. There are somewhere around 10,000 published papers per year on the
microbiome. That’s a tsunami. This paper … really puts a stamp that
this is where we need to look.”
Keeping Genetics in Perspective
Jamie Morton, a corresponding author of the Nature study, told The
Epoch Times that while there’s great data on how the environment shapes
the microbiome, genetics will always be valuable because they determine
how we’re influenced by toxic exposures.
He said that the study illustrates a cultural shift driving the
marriage of researchers who tend to “camp out” in their own disciplines
and are now uniting for the greater good of finding the cause of autism.
“That was one of the key points in our paper,” Mr. Morton said. “We
wanted to highlight that when we are thinking about autism and these
complex systems, you need everyone sitting in the same room. You need
not just one dataset. You need all of them. You need genetics. You need
microbiome. You need diet. You need metabolites, behavioral data,
everything you can get your hands on.”